Tags
deep vein thrombosis, Health, Lucknow, Preventive medicine, pulmonary embolism, Thrombosis, Thrombus, Vein
Deep vein thrombosis and pulmonary embolism following Orthopaedic Surgeries: Emerging trends in Prophylaxis and Anaesthetic consideration
a* b Aparna Shukla , Alpesh Shukla Contents lists available at CurrentSciDirect Publications; Journal homepage: http://www.currentscidirect.com
Int J Cur Biomed Phar Res. 2011; 1(3): 134-140
a* Associate Professor, Department of Anaesthesia, Rohilkhand medical college and hospital, Bareilly bConsultant Orthopaedic Surgeon, Krishna lifeline hospital, Lucknow
A B S T R A C T
 Orthopaedic illness and trauma in which patient remains unambulatory for prolonged period, predispose the patients to the occurrence of venous thromboembolic complications. These complications are predictable and are result of alterations of natural equilibrium in various disease states [1].
Orthopaedic illness and trauma in which patient remains unambulatory for prolonged period, predispose the patients to the occurrence of venous thromboembolic complications. These complications are predictable and are result of alterations of natural equilibrium in various disease states [1].
The incidence of deep vein thrombosis (DVT) is about 14% in gynaecological surgeries, 22% in neurosurgery, 26% in abdominal surgeries and 45-60% in patients undergoing hip and knee surgeries [2].
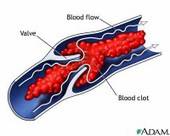
In high risk groups it is more cost effective to protect against DVT and pulmonary embolism (PE) than to treat these conditions when they occur. In this article we have discussed various mechanical and pharmacological prophylactic measures available, results of previous studies,and use of different anaesthesthetic techniques in the patients in whom prophylactic anticoagulant therapy is planned. Venous thrombi are different from arterial thrombi, in terms of their site of formation as well as in their appearance and make-up.
Arterial thrombi are pale-colored and rich in platelet count while venous thrombi are red, less compact and contain many red blood cells entrapped in fibrin network.
Rudolph Virchow in 1856 described the factors that predispose to DVT. These components are stasis, hypercoagubility and initimal injury.
The first component of the triad that is stasis,is as a result of venous pooling due to supine positioning and effects of anaesthesia.
The second component, hypercoaguability, occurs as a consequence of decreased clearance of procoagulant factors, with or without underlying coagulopathies.
The third component, initimal injury, results from excessive vasodilatation caused by vasoactive amines and anaesthesia. The combined influence of these factors promotes the development of venous thrombi in low flow areas. The propagation of thrombus leads to the development of overt DVT[3-9].
Related articles
- Be a Proactive Patient: Protect Yourself from Deep Vein Thrombosis (everydayhealth.com)
- Blood Clot Complications (everydayhealth.com)
- DVT Treatment Guidelines (everydayhealth.com)
- The Facts on Deep Vein Thrombosis (everydayhealth.com)
- YAZ / Yasmin / Ocella / Beyaz / Safyral: Drug Safety Regulators Focus On Blood Clot Side Effects (drug-injury.com)
- Father warns of blood clots from video gaming (ctv.ca)
- How long does it take to get the results from a leg venous doppler? (zocdoc.com)
- Anti-coagulant Blockbuster Drugs Are Here… (earlsview.com)
- DVT linked to video gamer’s death (bbc.co.uk)
- Videogame Marathons to Blame in Young Man’s Death (1up.com)

Pingback: Operative time, use of biological agents increase risk of complications following TKA « Earl's View
Pingback: Blood Clots – what you need to know « Earl's View
Pingback: Deep Vein Thrombosis, or DVT, can happen to anyone in an instant. « Earl's View
Pingback: Contralateral Deep Venous Thrombosis After Hip Arthroscopy « Earl's View